Table of Contents
The gut microbiome, made up of trillions of microorganisms, plays a crucial role in regulating not only digestive health but also mental well-being and immune function. In recent years, an increasing body of research has unveiled how these tiny inhabitants of the gut influence brain function and immune responses, opening the door to new ways of managing mental health and immune-related conditions. This article highlights five key insights into the relationship between gut bacteria, mental health, and immune responses.
1. The Gut-Brain-Immune Connection
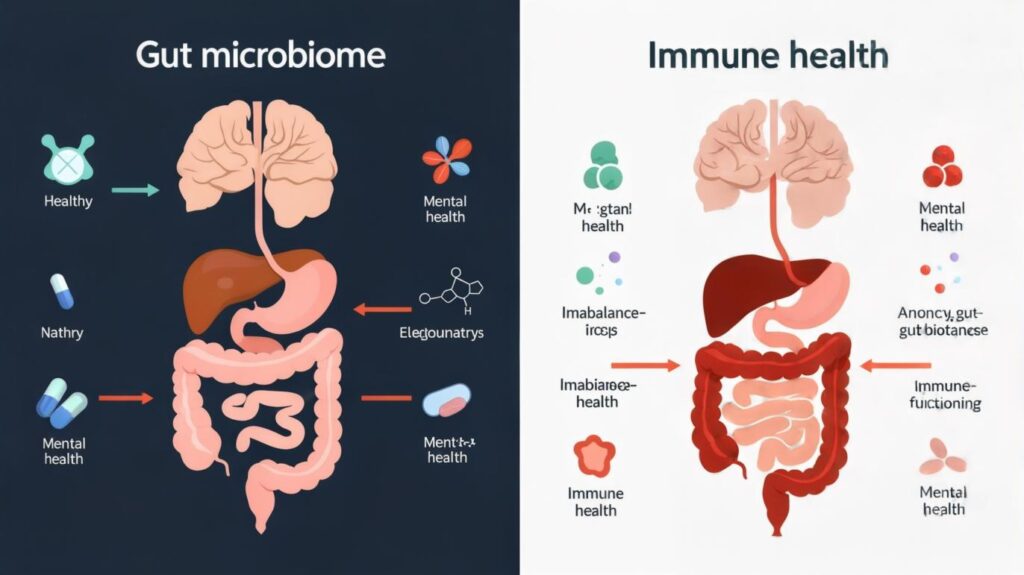
The term “gut-brain-immune axis” refers to the intricate and bidirectional communication network between the gastrointestinal tract, the brain, and the immune system. This connection is central to understanding how gut bacteria influence both mental health and immune function.
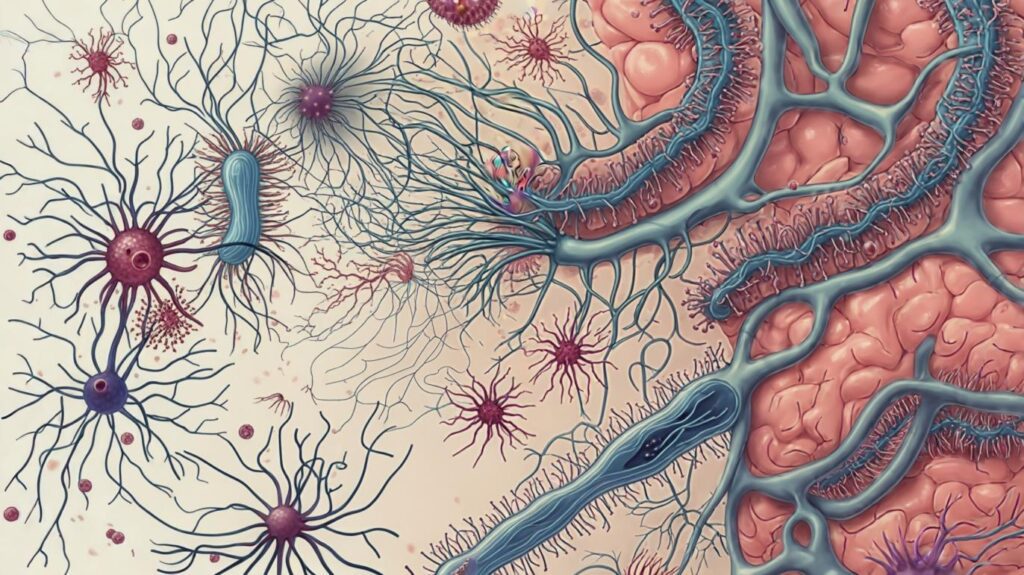
Gut bacteria interact with the brain through several key pathways, including neural, hormonal, and immune signaling systems. One of the most prominent pathways is the vagus nerve, a major communication route between the gut and the brain. The vagus nerve transmits signals about the state of the gut microbiome to the central nervous system, influencing mood, behavior, and cognitive processes. A well-balanced microbiome sends positive signals, while dysbiosis, or microbial imbalance, can interfere with these processes.
Moreover, gut microbiota directly interact with immune cells present in the gut-associated lymphoid tissue (GALT). These cells help regulate the body’s immune responses, affecting inflammation levels and systemic immunity. As gut bacteria communicate with both the brain and the immune system, they form a complex web that affects overall health.
2. The Role of Gut Bacteria in Mental Health Disorders
Research has shown that the composition of gut bacteria is closely linked to mental health. Dysbiosis—an imbalance of beneficial and harmful bacteria in the gut—has been implicated in the development of mental health disorders such as depression, anxiety, and schizophrenia.
A reduction in microbial diversity or the dominance of certain pathogenic species in the gut has been observed in people suffering from these conditions. For example, individuals with depression often have lower levels of beneficial bacteria like Bifidobacterium and Lactobacillus, while pathogenic bacteria such as Firmicutes and Bacteroidetes may dominate.
Gut bacteria influence mental health in several ways. They produce a variety of metabolites, including short-chain fatty acids (SCFAs), which are critical for maintaining the integrity of the blood-brain barrier and modulating inflammation in the brain. Additionally, gut bacteria are involved in the production and regulation of neurotransmitters like serotonin, which is primarily produced in the gut and plays a key role in mood regulation. Disturbances in these processes may contribute to mood disorders.
Emerging therapies targeting the gut microbiome, such as the use of probiotics and prebiotics, are showing promise in managing mental health conditions. Studies have found that restoring a balanced microbiome through probiotic supplements or dietary changes can help alleviate symptoms of depression and anxiety.
3. The Impact of Gut Bacteria on Immune Function
The gut microbiome is not only vital for mental health but also plays a fundamental role in regulating immune function. A significant portion of the body’s immune system is located in the gut, specifically in the GALT. Here, gut bacteria interact with immune cells, helping to shape the immune system’s response to pathogens, infections, and inflammation.
A healthy microbiome supports the development of a balanced immune system by promoting the production of anti-inflammatory molecules and preventing excessive immune responses that can lead to chronic inflammation. In contrast, dysbiosis can disrupt this balance, leading to immune dysfunction and increasing the risk of autoimmune diseases, such as rheumatoid arthritis and inflammatory bowel disease (IBD).
Chronic low-grade inflammation, often caused by a disrupted gut microbiome, is also associated with several mental health conditions, including depression and anxiety. This inflammation can affect the brain’s neurotransmitter production, further complicating mental health symptoms. Thus, maintaining a balanced gut microbiome is crucial for both immune function and mental well-being.
4. The Science Behind Gut-Produced Neurotransmitters
A fascinating aspect of the gut-brain connection is that gut bacteria play a direct role in the production and regulation of neurotransmitters. For example, around 90% of the body’s serotonin, a neurotransmitter involved in regulating mood, is produced in the gut. The gut microbiota influence serotonin synthesis by producing certain metabolites that affect serotonin-producing cells in the intestines.
In addition to serotonin, gut bacteria also play a role in the production of other important neurotransmitters, including dopamine and gamma-aminobutyric acid (GABA). These chemicals help regulate mood, cognition, and emotional responses. Disruptions in the balance of these neurotransmitters, often due to imbalances in gut bacteria, have been linked to conditions like anxiety, depression, and even schizophrenia.
The discovery of this gut-brain interaction has led to innovative research into how modifying the gut microbiome could potentially offer therapeutic options for treating mental health disorders. Probiotics, for instance, may help normalize neurotransmitter levels, potentially reducing symptoms of conditions like depression and anxiety.
5. Therapeutic Approaches to Modulating the Gut Microbiome
Understanding the influence of gut bacteria on mental health and immune responses has opened new therapeutic avenues. Modulating the gut microbiome through dietary interventions, probiotics, prebiotics, and even fecal microbiota transplantation (FMT) is an emerging field in medicine.
- Probiotics and Prebiotics: Probiotics are live beneficial bacteria that help restore balance to the gut microbiome, while prebiotics are non-digestible fibers that support the growth of these beneficial microbes. Incorporating probiotic-rich foods, such as yogurt, kefir, and fermented vegetables, along with prebiotic-rich foods like garlic, onions, and bananas, can enhance gut health and improve mental and immune function.
- Dietary Interventions: A diet rich in fiber, polyphenols, and omega-3 fatty acids supports gut health. Studies have shown that fermented foods like kimchi, sauerkraut, and miso can have a positive impact on both the gut microbiome and mental health. Foods rich in omega-3s, such as fish and flaxseeds, can also help reduce inflammation and improve brain health.
- Fecal Microbiota Transplantation (FMT): FMT involves transferring fecal matter from a healthy donor into a recipient to restore a healthy gut microbiome. While FMT is most commonly used to treat Clostridium difficile infections, emerging research suggests that it may also have benefits for mental health disorders. For example, some studies have shown that FMT can reduce symptoms of depression and anxiety in patients with dysbiosis.
Conclusion
Gut bacteria have an undeniable influence on mental health and immune responses. Through the gut-brain-immune axis, these microorganisms regulate neurotransmitter production, modulate immune function, and even impact mood and cognitive processes. Maintaining a healthy and diverse gut microbiome is critical for overall well-being, and therapeutic interventions targeting the microbiome, such as dietary changes, probiotics, and FMT, are showing promise in supporting both mental and immune health. As research continues to unfold, it is likely that personalized microbiome-based treatments will play a larger role in healthcare strategies aimed at improving mental health and immune function.